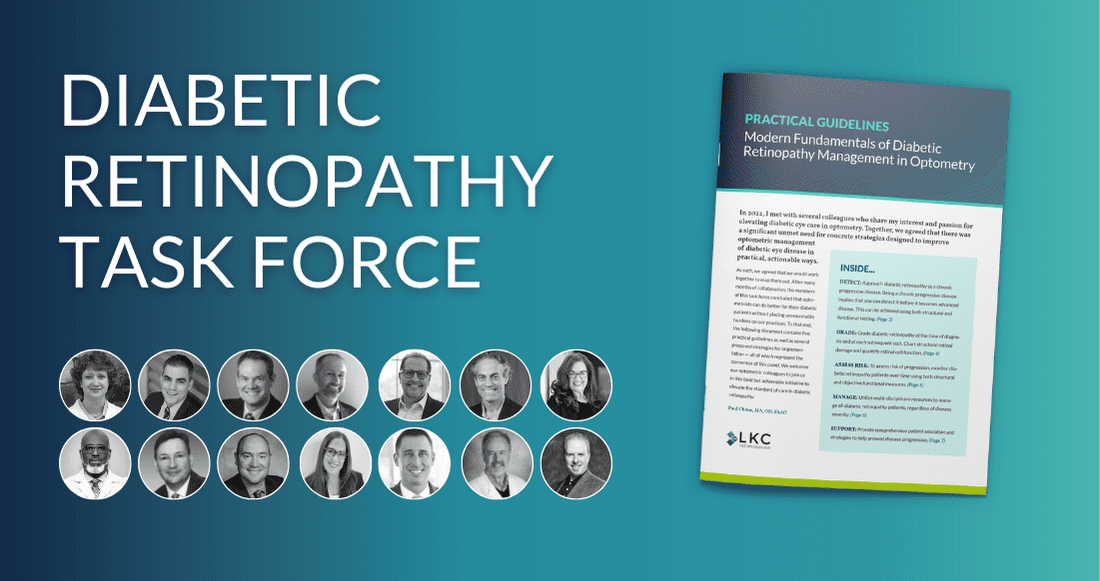
Collaboration to Elevate the Standard of Care for Diabetic Retinopathy
By Paul Chous, MA, OD, FAAO, Michael Cymbor, OD FAAO, Jeffry Gerson, OD, FAAO, Dorothy Hitchmoth, OD, FAAO, Paul Karpecki, OD, FAAO, Nate Lighthizer, OD, FAAO, and Bobby “Chip” Wood, OD.
Why did you join the diabetic retinopathy task force and what has the group achieved?
Dr. Chous: In 2022, I met with several colleagues who share my interest and passion for elevating diabetic eye care in optometry. We all agreed that there was a significant unmet need for concrete strategies to improve optometric management of diabetic eye disease. This unmet need in our profession creates a lot of variation in patient care and, ultimately, in patient outcomes. We formed a task force with a goal of creating actionable, practical guidelines to help address this significant public health issue.
Dr. Wood: We absolutely needed some basic guidelines and concrete strategies that standardize how we meet the growing patient need.
Dr. Lighthizer: After many months of collaboration, we concluded that optometrists can do better for their patients without placing unreasonable burdens on our practices. To that end, the report (Fundamentos modernos del tratamiento de la retinopatía diabética en optometría) contains five practical guidelines as well as several proposed strategies for implementation — all of which represent the consensus of the full panel.
Dr. Karpecki: In short, optometrists need to 1) detect, 2) grade, 3) assess risk, 4) manage and 5) support. (See Five Pillars of DR Management below)
Dr. Hitchmoth: Some would argue that a dilated fundus exam and visual acuity check tick the box, but in my experience, it’s not enough. In many cases, these basics don’t give us the confidence to say that we’re doing all we can for patients. We need to approach diabetic retinopathy as a chronic progressive disease.
Five Pillars of Diabetic Retinopathy Management
Dr. Wood: Exactly. And being a chronic progressive disease implies that you can detect it before it becomes advanced disease. The question is, how do we do this?
Dr. Chous: To begin, we need to use both structural and functional testing. OCT-A is a real game changer in structural testing. And on the functional side, although the standard of care for the assessment of vision loss due to diabetic retinopathy is high-contrast visual acuity, evidence shows it is insufficient.
Dr. Hitchmoth: I advocate for electro-diagnostic testing (ERG), preferably utilizing the additional measure of pupillometry, as in the DR Score offered by the RETeval®.
Dr. Gerson: This test is non-invasive and entirely objective, providing a simple score that indicates whether my patient may be in trouble. This is achieved by measuring both retina cell stress and pupil light response. This powerful combination provides a reliable progression risk assessment.
Dr. Cymbor: As patients worsen into moderate and severe nonproliferative disease, it may become challenging to determine the best time to refer to a retinal specialist. The DR Assessment Protocol helps me to clarify the correct time to refer, enhancing patient outcomes. A score of 23.5 or higher indicates an 11-fold risk of requiring intervention within 3 years.1