Estudo de Caso
A Tale of Two Patients: How ERG Uncovered Hidden Differences
by Kelly MacDonald, OD

Patient History
Patient 1
Two diabetic retinopathy (DR) patients presented to my office on the same day. Patient 1 was a 63-year-old male who was presenting for follow-up for bothersome dry eye symptoms and mild DR with macular edema. He is also a glaucoma suspect. The patient was diagnosed with diabetes at age 37. His HbA1c is 6.0. His BCVA is stable at 20/20 OD 20/25 OS. The dilated retinal exam revealed a few scattered dot and blot hemorrhages in both eyes, which are difficult to appreciate on the Optomap (Figure 1).
Patient 2
Later this same morning, another mild DR patient presented for follow-up. This 55-year-old male was also diagnosed at age 37 and had a slightly higher HbA1c of 9.1. However, this second patient has no history of macular edema. Like Patient 1, Patient 2 had not noticed any visual changes and had a BCVA of 20/20 OD and 20/25 OS.
The dilated retinal exam for Patient 2 showed scattered dot and blot hemorrhages OU and there was an area of myelinated NFL superior OD that had hemes within the myelination (Figure 3). In fact, there were several dot hemes in the macula of each eye, but otherwise his retinopathy had been quite stable since his previous exam.
Figure 1: Patient 1 Fundus Exam

Figure 3: Patient 2 Fundus Exam

The OCT revealed a very mild area of macular edema in the right eye and an unremarkable left eye appearance (Figure 2).
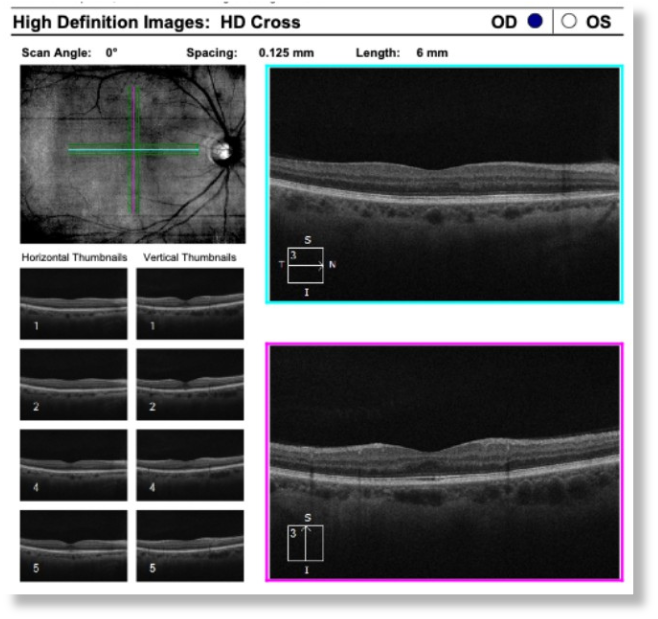
The OCT was unremarkable OD, but I noted mild cystic changes OS, which indicated very early, mild macular edema (Figure 4).
Figure 2: Patient 1 OCT
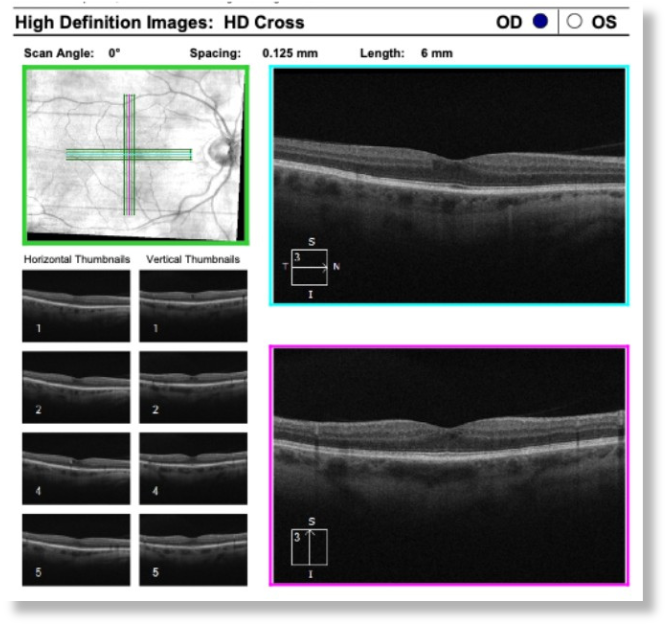
Figure 4: Patient 2 OCT
Why Was the ERG Performed?
These patients presented back-to-back very soon after I acquired a RETeval device in my practice. In fact, I had only just recently started to grasp and appreciate the clinical applications of ERG and the implications that these findings could have in my day-to-day practice. When I was thinking about whether to add an ERG device, it was patients just like these two who I intended to test, so it was quite a coincidence that they presented close together on the same day. Overall, I wanted more complete information about my patients with diabetes so I could more confidently follow them over time and determine appropriate follow-up visit intervals.
What Were the ERG Findings?
Patient 1
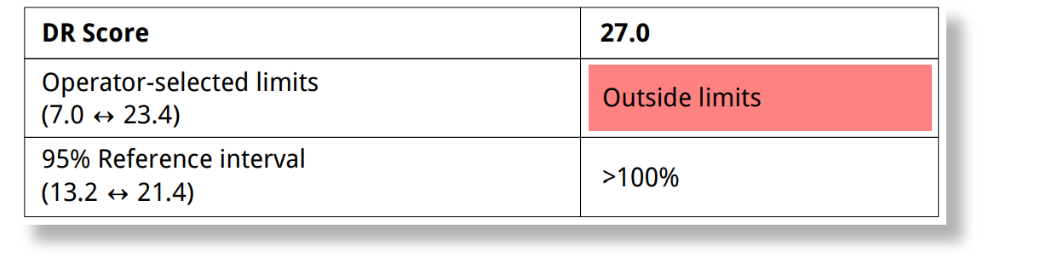
Patient 1 had a DR Score of 17 (Figure 5), which helped explain how macular edema could persist for three years yet not progress to treatment. Patients like this can make you feel uneasy and cause worry that you’re missing something, but the ERG fills those knowledge gaps and, in this case, revealed that the patient’s retina was not overly stressed despite the chronic edema.
Patient 2
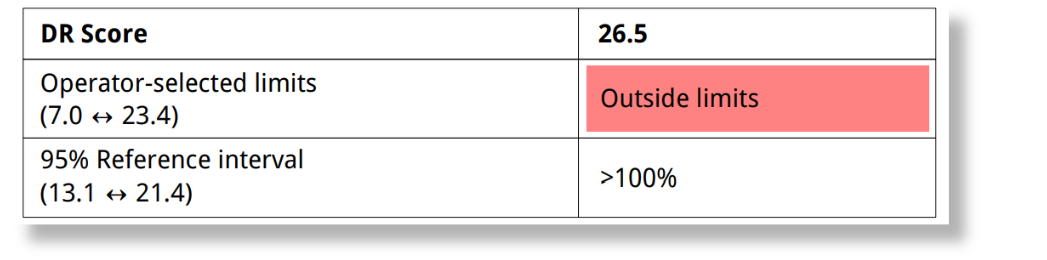
Despite similar OCT findings relative to Patient 1, Patient 2 had a DR Score of 27 (Figure 6), which was disconcerting since he had been stable for several years with no notable progression of disease that I could detect or document prior to this initial ERG.
Figure 5: Patient 1 ERG

Figure 6: Patient 2 ERG
How Did the ERG Impact Next Steps?
Patient 1
Given the normal DR Score for Patient 1, I felt safe with a 6-month follow-up. Conversely, I was now more worried about Patient 2 and shortened his follow-up interval to 3 months.
Patient 2
At that 3-month follow-up visit for Patient 2, I learned that he lowered his HbA1c for the first time in almost 20 years and his DR Score also decreased from 27.0 to 26.5 (Figure 7). He asked me if he could go back to 6-month visits if he continues to maintain better control. Although I am not yet comfortable stretching out the visits, I am encouraged that the DR score provided much-needed motivation for the patient.
Figure 7: Patient 2 Follow-up ERG
This case was billed as follows, based on medical necessity:
- Patient 1: E11.3213 type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy with macular edema, bilateral.
- Patient 2: E11.3293 type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema, bilateral.
Why We Use RETeval
While the research on ERG is what initially motivated me to bring it into practice, seeing how it has a real impact on patient management daily has made me so grateful to have this tool at my disposal. Performing ERGs on back-to-back patients who I would otherwise have managed identically delivered a “wow” factor that I was not expecting. RETeval truly impacted patient care immediately.
Practice Protocol
My goal is to use the RETeval to enhance patient care by providing clarity in complicated cases. To that end, I use ERG for patients with diabetic retinopathy, macular degeneration, optic nerve issues (edema, atypical cupping, atrophy, etc.), and cases where the diagnosis is in question and information about retinal function will be clinically useful. O ERG testing is performed by our technicians as part of a testing schedule that also includes OCT and visual fields.

Kelly MacDonald, OD
Focused Eye Care (Nashua, NH)
Dr. MacDonald earned her degrees at the New England College of Optometry, where she received numerous academic awards and volunteered extensively. She is a member of both the American Optometric Association and the New Hampshire Optometric Association, a long-time member of the Rotary Club of Nashua, and has been voted “Best Optometrist” in the greater Nashua area multiple times in recent years by readers of the Nashua Telegraph.



