Estudo de Caso
ERG Raises Red Flag, Changing Management Trajectory
by Frances Bynum, OD
A complaint of difficulty driving at night is not uncommon for an optometrist to hear, but when one patient mentioned this during his routine exam, his visual acuity of 20/20 signaled Dr. Frances Bynum, OD, FAAO, to look further. Fundus and auto fluorescence imaging showed pigment changes and retinal defects, leading Dr. Bynum to order an ERG with the RETeval. Despite an unchanged visual acuity, the patient’s retina function was severely compromised. Dr. Bynum then leveraged this data and the RETeval’s color-coded report to better explain her findings to the patient and guide next steps when making a referral to a retina specialist for her diagnosis of sector retinitis pigmentosa.
Watch the video of Dr. Bynum presenting her case or review the case below.
Patient History
A 46-year-old Caucasian male with no family history of retinal or other concerning ocular disease presented for a routine exam. His visual acuity was 20/20 in both eyes. The only complaint that he had was some difficulty driving at night. He noted that it was challenging to see under these conditions.
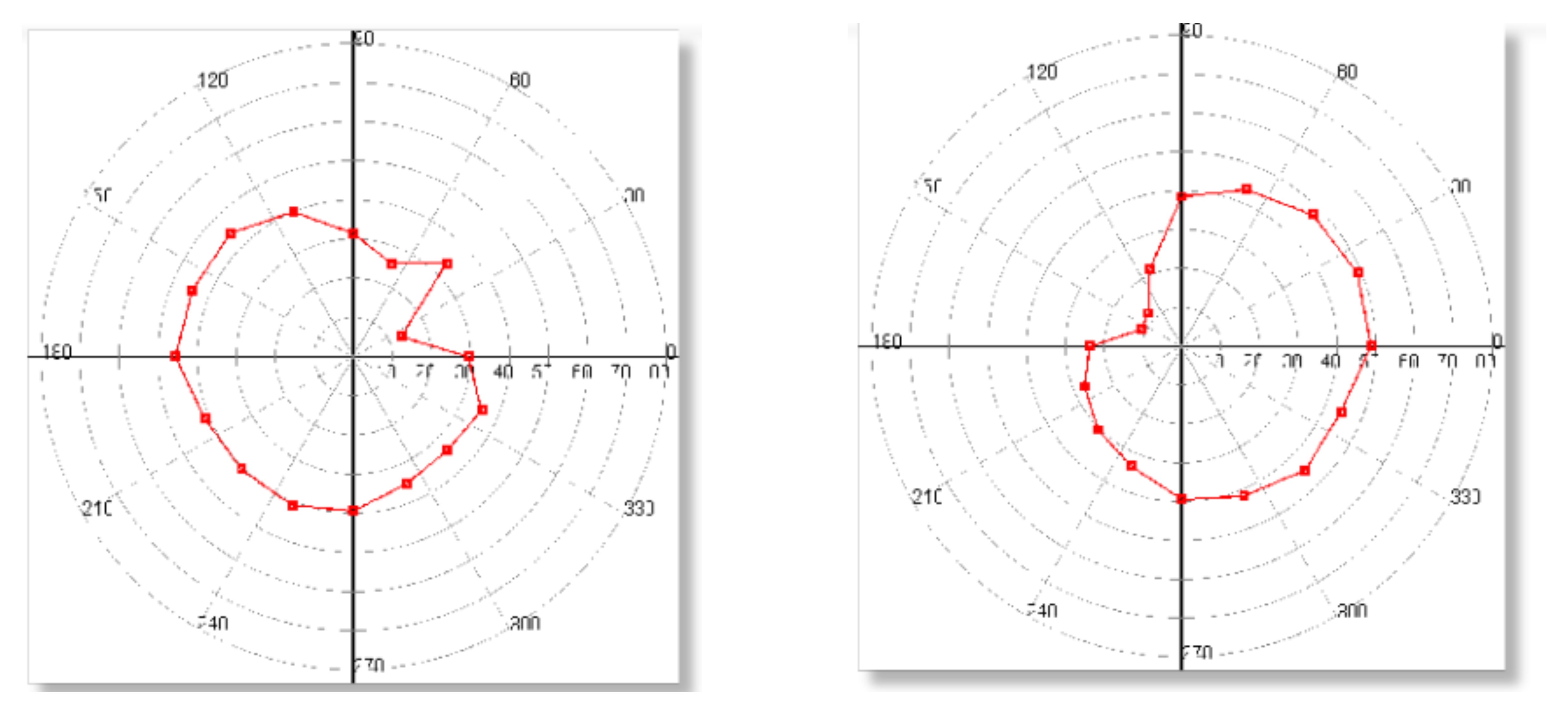
Fundus examination revealed some pigment changes nasally on both eyes (Figure 1). Upon further investigation, I realized that these were mild bone spicules, so we proceeded to capture auto fluorescence images. As the FAF images show, the patient had quite a bit of retinal loss in the nasal aspect of both retinas (Figure 2). A visual field further confirmed the presence of the nasal defect (Figure 3).
Figure 1:
Fundus OD Fundus OS
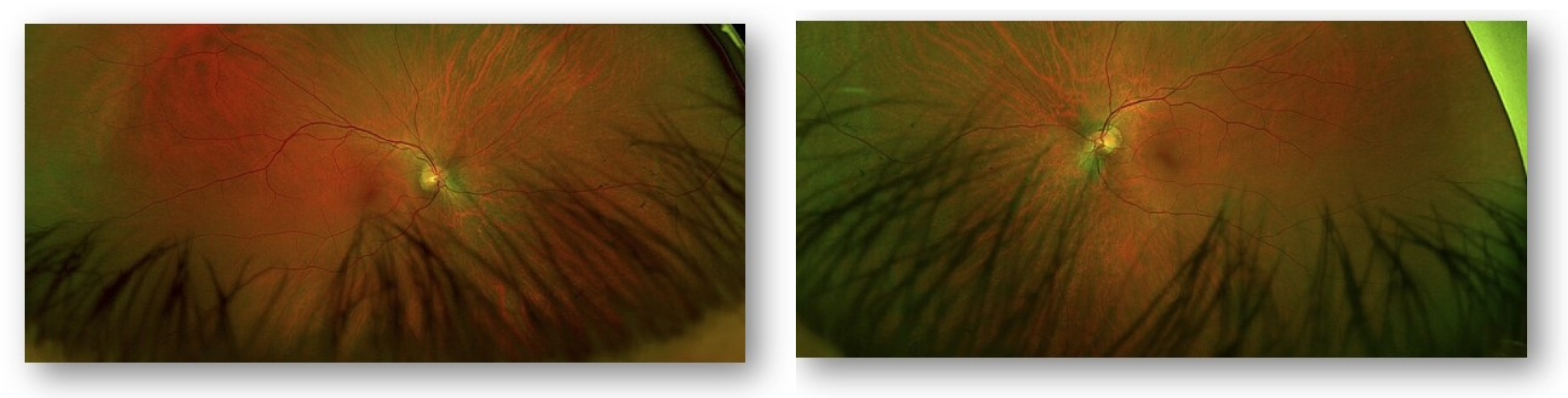
Figure 2:
Auto Fluorescence OD Auto Fluorescence OS
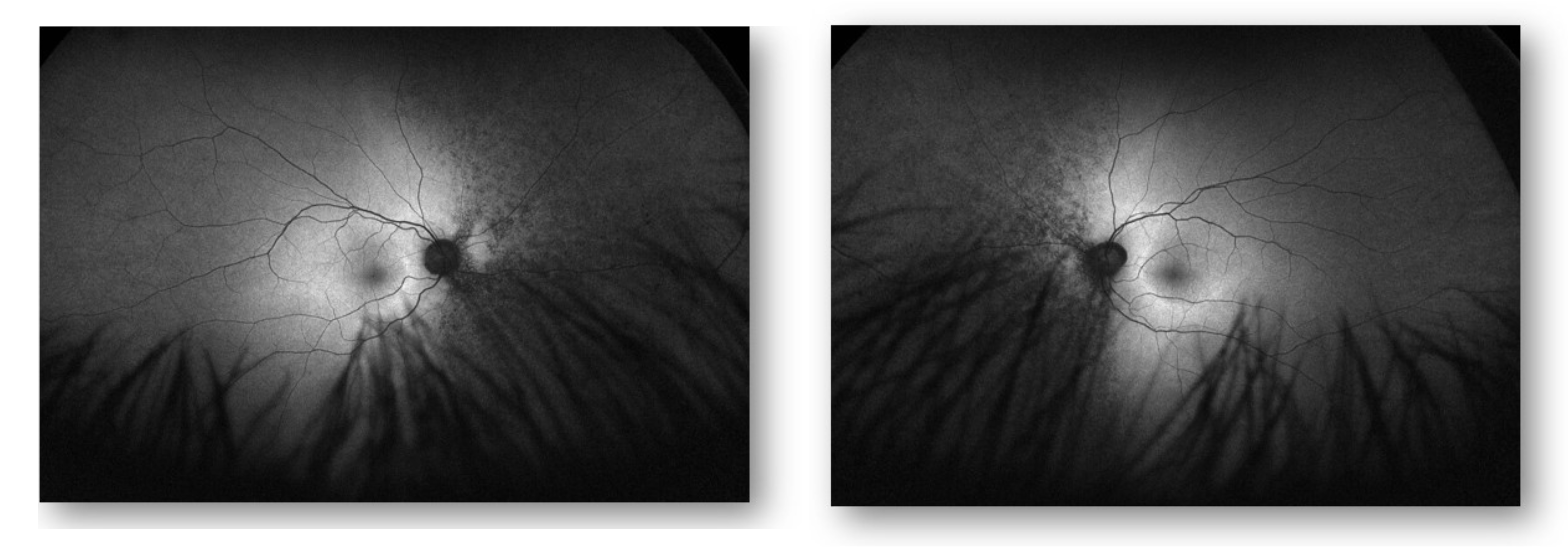
Figure 3:
Visual Field OD Visual Field OS
Why Was the ERG Performed?
We felt it was important to get a better understanding of the patient’s functional deterioration in this case. We wanted the ERG results to help paint a picture that would make it easier to explain the findings to the patient and guide next steps when making a referral to the retinal specialist.
What Were the ERG Findings?
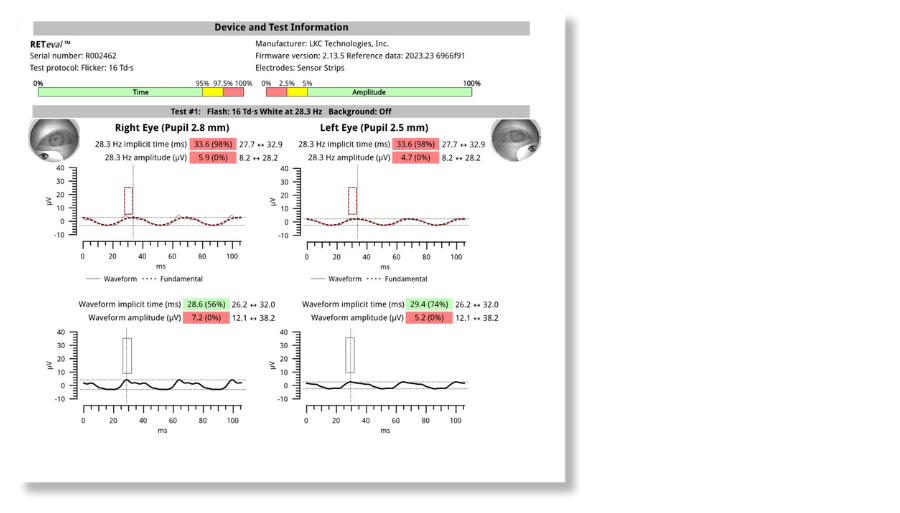
The Flicker 16 protocol (Figure 4) showed significantly decreased amplitudes and implicit times. The fundamental waveform was used in this instance due to the extremely low amplitudes. Importantly, the ERG also indicated that there is more severe functional vision loss than the visual field or the visual acuity represent in this case. Based on the combination of testing that was performed, I correctly suspected the patient had sector retinitis pigmentosa and made referrals for additional testing with a specialist.
Figure 4:
How Did the ERG Impact Next Steps?
RETeval testing prompted us to initiate important next steps, which included blood work for genetic testing. ERG also provided the information needed to determine eligibility for clinical trials that this patient may benefit from in the months ahead. Currently, there is no treatment for retinitis pigmentosa, but making the correct diagnosis and being able to direct my patient to the right specialists and services may be very helpful in the future — not only for himself, but for any children that he might have.
Finally, what I really liked about the ERG in this case was the color-coded print out of the results. This made it much easier to sit down and go over the findings with the patient. We talked about potential progression as well as his driving issues. I explained that he should refrain from driving at night or in low light conditions, such as cloudy or rainy days.
This case was billed using E11.329 – diabetes with mild non-proliferative retinopathy w/o macular edema based on medical necessity.
Why We Use RETeval
O teste PhNR do RETeval device makes me a better diagnostician and boosts my confidence managing disease progression. With ERG, I can monitor retinal function objectively, rather than relying too heavily on tests that require subjective patient responses.
Practice Protocol
When we first acquired the RETeval device, we focused on DR. We ran a DR Assessment on all patients who had both diabetes and signs of retinopathy. My technicians quickly learned how to use the RETeval, and it was so simple to implement into the practice flow. Because it’s portable and patients don’t have to move from room to room, we were able to start using the device on a variety of patients in whom structure and function was not really matching up. Now we have protocols for a host of diseases such as retinal vascular diseases, optic nerve disease including glaucoma and any unexplained vision loss in cataract patients.

Frances Bynum, OD
Northwest Tennessee Eye Clinic (Martin, TN)
Dr. Bynum is a Vision Source administrator and owner of a solo practice in a rural market. Her technical expertise has afforded her the ability to bring state-of-the-art procedures and technology into her practice, allowing patients to obtain a comprehensive range of services close to home. She’s a patient education advocate and believes that she and her patients can manage blinding eye diseases best when working as a team.



