Estudo de Caso
The Predictive Value of Combining Diagnostic Technologies
by A. Paul Chous, MA, OD, FAAO
Paul Chous, an optometrist in Tacoma, WA, leveraged his RETeval‘s predictive Diabetic Retinopathy Score along with OCT-A technology to determine that, despite normal fundus and OCT, a four-month follow-up was the most appropriate course of action for his patient with an 18-year history of type 1 diabetes – a decision that was reaffirmed when the patient presented with rapidly worsening proliferative diabetic retinopathy (PDR) at his next appointment. In this case presentation, Dr. Chous explains how this combination of diagnostic modalities led to crucial intervention that would have otherwise been missed.
Watch the video of Dr. Chous presenting his case or review the case below.
Patient History
A 39-year-old Caucasian male with an 18-year history of type 1 diabetes mellitus (T1DM) presented for a comprehensive exam. His medications included insulin aspart (60-80 units daily) and 150 mcg of levothyroxine for Hashimoto’s thyroiditis.
He is on continuous subcutaneous insulin infusion (CSII) via a pump and he also takes an extra bolus of insulin with meals. His HbA1c has improved steadily, with a range 6.4% to 12.7%. He wears a continuous glucose monitor (CGM) and has achieved a 90-day time-in-range (TIR) of 64%. In other words, his blood sugars have been within a relatively normal range [70-180 mg/dL] 64% of the time. We generally set a goal of 70% for most patients. Interestingly, when I reviewed the data further, I discovered that he had hypoglycemia about 15% of the time, whereas the goal is typically < 4% of the time.
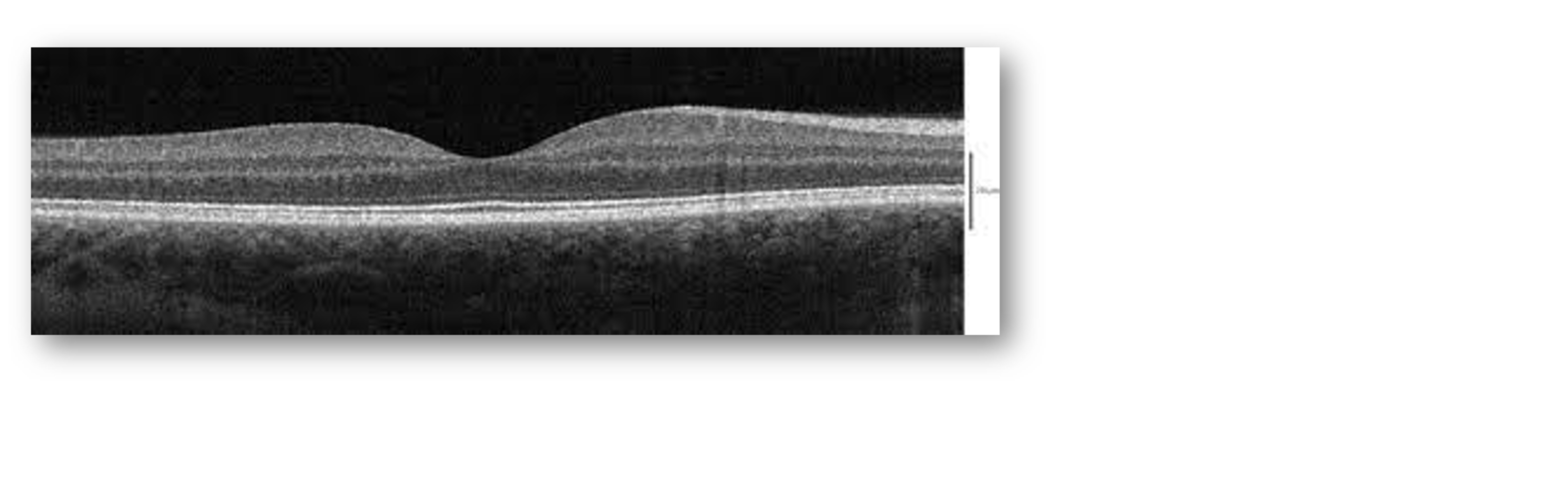
At the baseline exam, best corrected visual acuity was 20/20 OU, with normal pressures. I noted that he had mild non-proliferative diabetic retinopathy (NPDR), with a few microaneurysms that are barely evident on the fundus exam photos (Figure 1). Furthermore, the patient’s OCT looked normal (Figure 2).
Figure 1: Fundus Exam
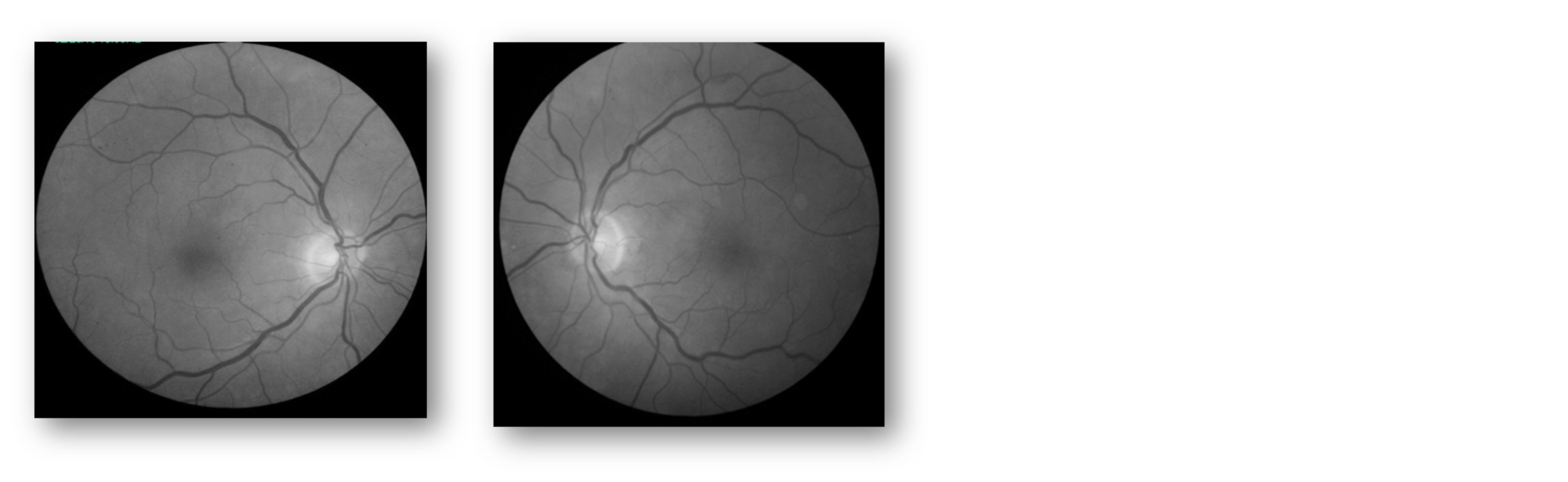
Figure 2: OCT
Why Was the ERG Performed?
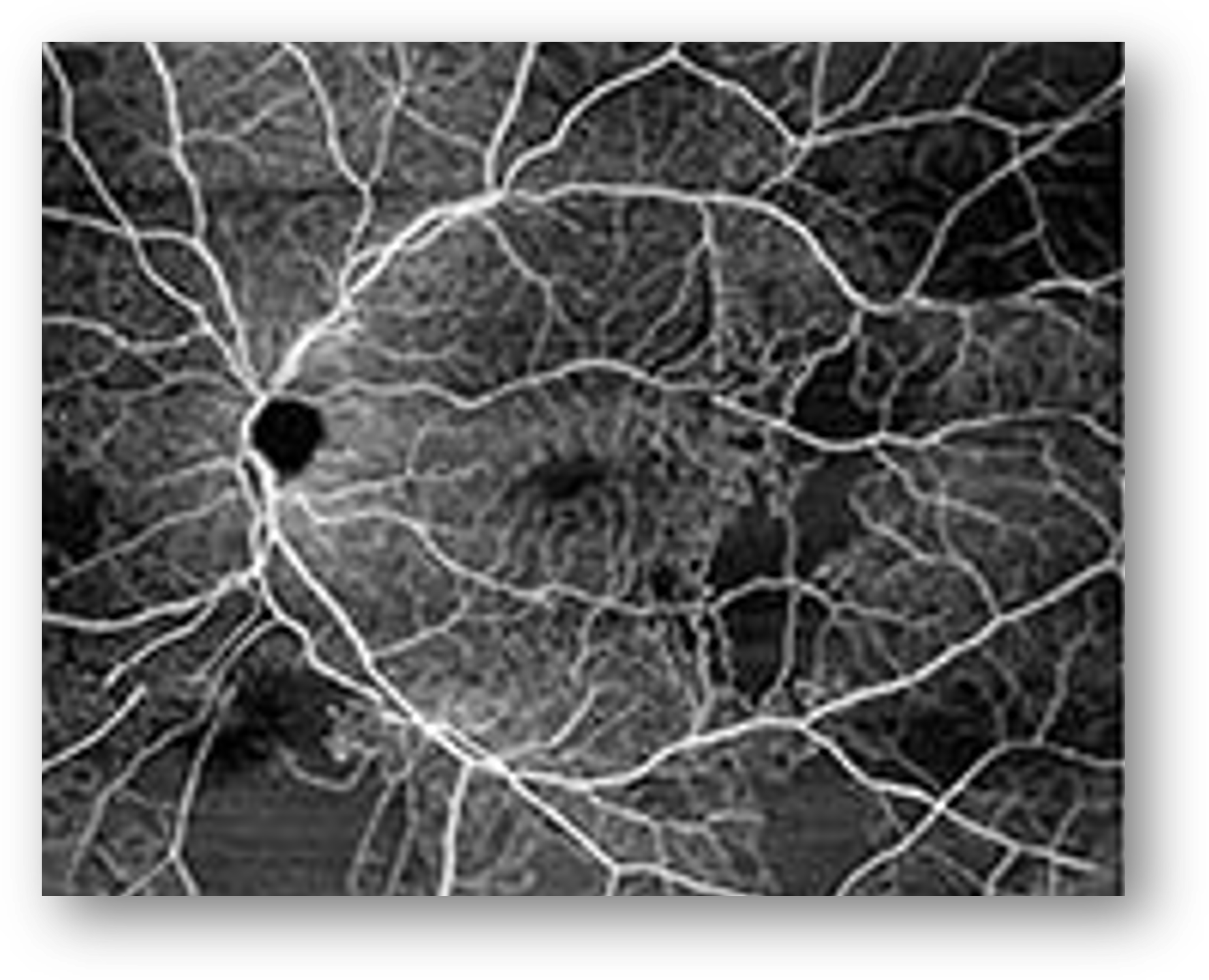
Despite the minimal NPDR depicted in the fundus photos and a normal OCT, we ran an OCT-A on the patient and found reason for concern in the left eye. Here, we noted significant patchy areas of non-perfusion and an irregular foveal avascular zone (Figure 3). That said, there was no evidence of intraretinal microvascular abnormalities (IRMA) or proliferative diabetic retinopathy (PDR). In cases like this, we want to learn as much as we can about the patient’s risk and therefore ran a baseline ERG next.
Figure 3: OCT-A
What Were the ERG Findings?
The ERG returned an abnormal DR Score of 25.5 (Figure 4), indicating that the patient is at high risk of requiring a retinal intervention in the next 36 months. Looking more closely, we also see that the b-wave amplitude is at the lower end of the normal range and the patient has reduced implicit times, which indicate retinal stress.
Figure 4: ERG
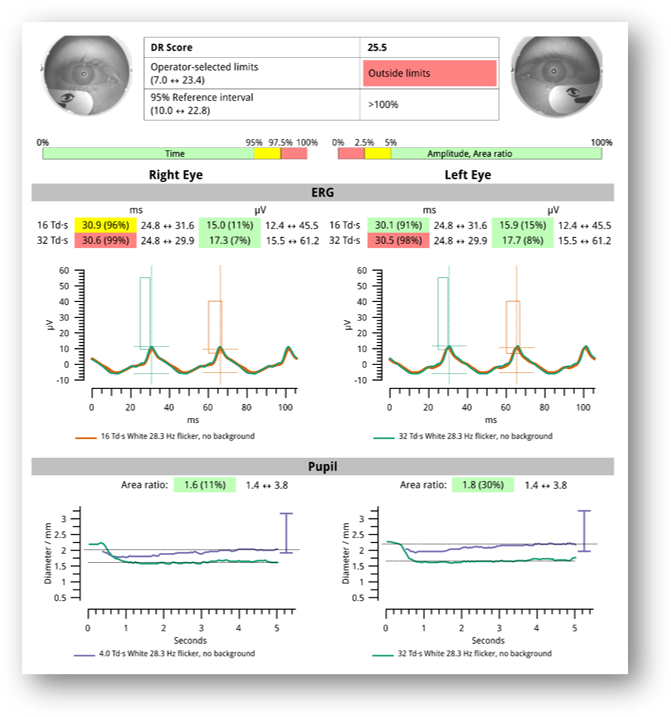
How Did the ERG Impact Next Steps?
If we had only had access to information from the fundus exam/photos and OCT, which showed mild NPDR without any diabetic macular edema (DME), we would have been comfortable with a longer follow-up. However, the areas of non-perfusion on OCT-A combined with the reduced retinal function on ERG made it essential to see the patient back sooner than we otherwise would have [4 months].
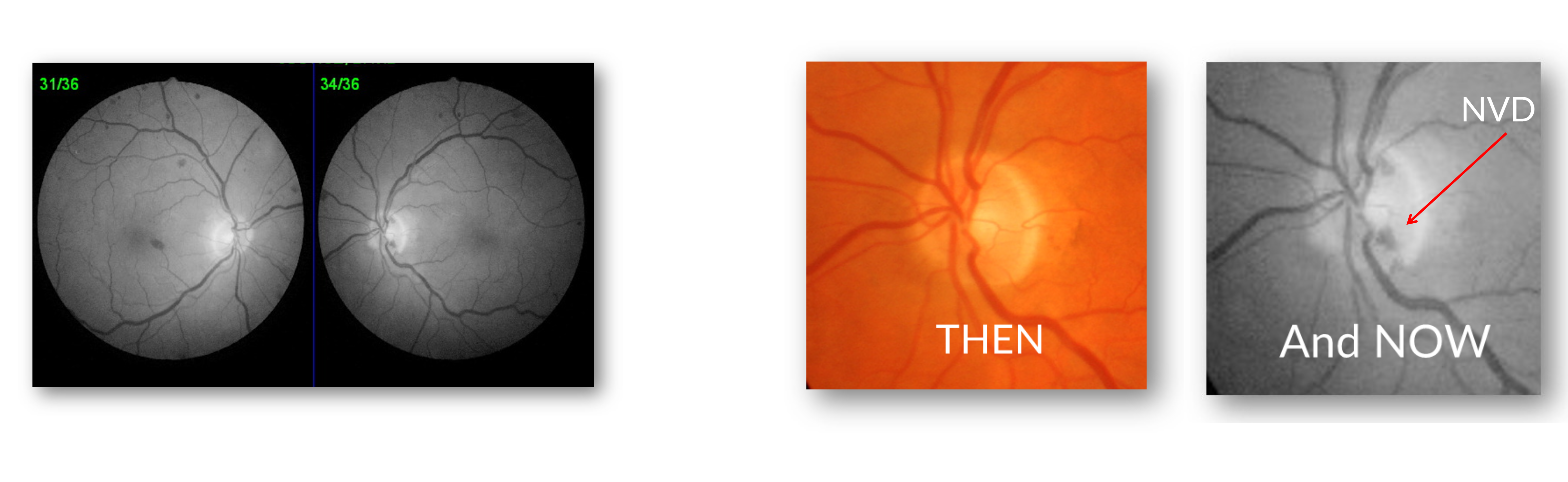
At the four-month follow-up, we discovered rapidly worsening DR with incident optic nerve neovascularization in the left eye. In fact, the difference in four month’s time is remarkable when you look at the photos side by side (Figure 5). I diagnosed the patient with PDR and referred him to a retinal specialist.
This case clearly demonstrates the value of combining diagnostic modalities for risk stratification in patients with diabetes and retinal disease. With ERG, I was able to detect sight-threatening retinopathy earlier than I would have otherwise.
Figure 5: Fundus Photography
This case was billed using the following based on medical necessity:
- Initial visit: E10.329 – type 1 diabetes with mild NPDR without macular edema.
- Follow-up visit: E10.3592 – type 1 diabetes with proliferative diabetic retinopathy without macular edema, left eye.
Why We Use RETeval
We use RETeval in our practice because it helps us to better clarify DR patients’ retinal status and, more importantly, their risk of progression to sight-threatening disease, especially when combined with structural findings as in this patient. It’s quick, easy, objective and predictive.
Practice Protocol
I’ve used the RETeval in my diabetes specialty practice since 2023. We collect a DR Score on all patients with known diabetic retinopathy of any severity. More recently, I have also started to test glaucoma patients and glaucoma suspects.

Paul Chous, MA, OD, FAAO
Chous Eyecare Associates (University Place, WA)
Dr. Chous is a diabetes eye care champion, author of the book Diabetic Eye Disease: Lessons from a Diabetic Eye Doctor, and has published more than 100 papers on diabetes. He’s an experienced, passionate speaker on the topics of diabetes, diabetic retinopathy, macular degeneration, and the role of nutrition in the eye. A diabetic since 1968, Dr. Chous knows first-hand what his patients need.



