Case study
ERG Alters Follow-up Schedule and Education for Patient with Diabetes
by Nate Lighthizer, OD, FAAO
When faced with non-proliferative diabetic retinopathy, many optometrists recommend annual follow-ups to continue monitoring disease progression. Nate Lighthizer, OD, FAAO, an optometrist and faculty member at the Northeastern State University Oklahoma College of Optometry, relies on the RETeval handheld ERG’s DR Assessment not only for its patient education benefits, but also for the enhanced progression risk analysis it offers.
Watch the video of Dr. Lighthizer presenting his case or review the case below.
Patient History
A 33-year-old Native American female with a history of diabetes presented because she lost her glasses a year prior. From a visual standpoint, she was doing well. She didn’t report any changes in her vision and was corrected to 20/20 in both eyes (-1.25 OD, -1.00 OS). Her last A1c was 10.0, which is certainly higher than we would like to see.
The fundus photos (Figure 1 and Figure 2) show increased hemorrhaging in both eyes when comparing the most current exam to an exam performed the previous year.
Figure 1: Fundus image (OD)
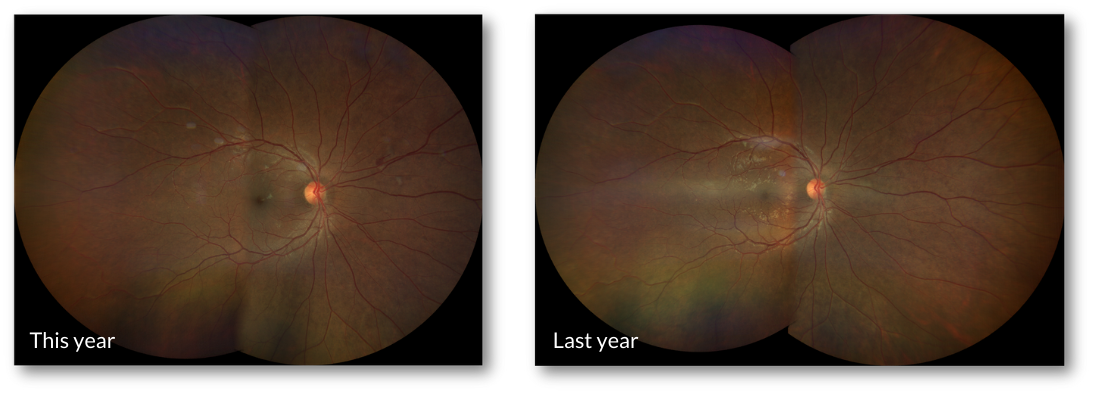
Figure 2: Fundus image (OS)
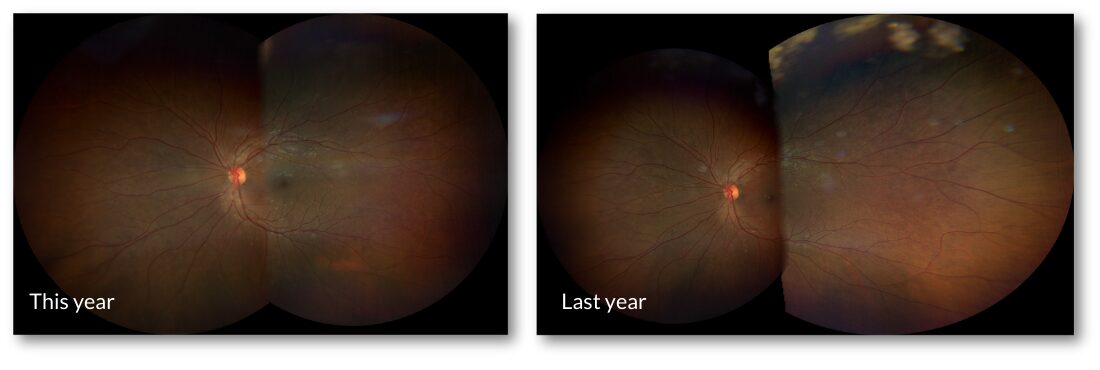
The photos show some progression, so we ran an OCT (Figure 3), which looks good overall, with no macular edema, no major macular ischemia or thinning.
Figure 3: OCT
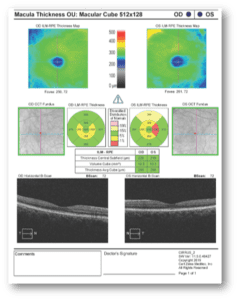
Given the history, systemic, and structural findings, I would classify this case as mild NPDR in a young patient with uncontrolled A1c. Based on this, I would say the patient needs to return for follow-up in one year. However, we now have access to a DR Score with the RETeval®, which can provide additional information.
Why Was the ERG Test Performed?
When managing patients with diabetes, especially when you see progression, but disease is still mild, the RETeval can offer a higher level of confidence to determine when a patient needs to be seen again.
My practice protocol is to perform ERG on all patients with diabetes if I see any degree of structural change, if the patient is uncontrolled, if there are recent vision changes, or if the patient has had diabetes for more than 5 years. Two of the four conditions applied here, so I didn’t think twice about the need to perform this test.
Patients also appreciate knowing their Diabetic Retinopathy Score because it provides the feedback they need to feel more in control of their health outcomes. Patients come back visit after visit wanting to compare their scores. We explain that anything above 23.4 is abnormal, so the lower they can get the score, the better.
What Were the ERG Findings?
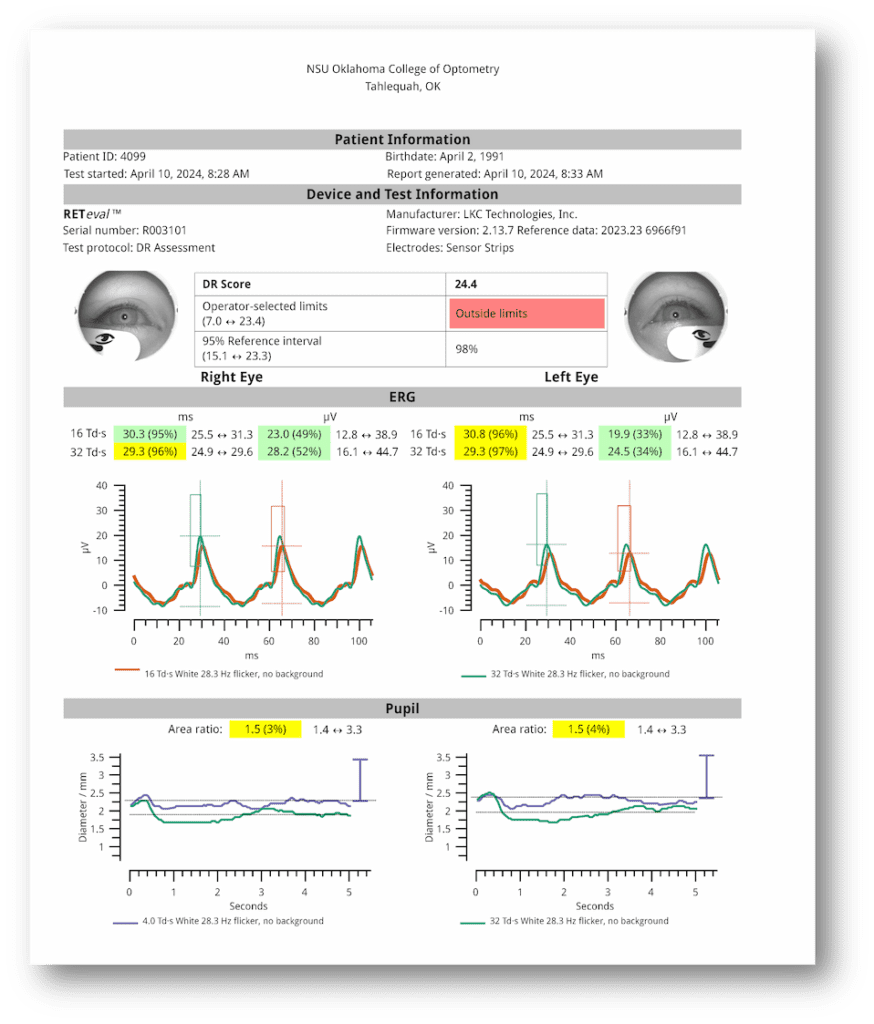
Although I would still classify this patient as having mild NPDR, the DR Score was abnormal at 24.4 (Figure 4), which indicates that this patient is more likely to progress to needing treatment.
Figure 4: ERG report with the DR Assessment protocol test results
How Did the ERG Impact Next Steps?
Due to the elevated DR Score indicating a higher risk of progression, I no longer feel comfortable waiting 12 months to see this patient back. Instead, I want to set the next follow-up to four months and then potentially move to six months. This will give me an opportunity to have more of a show-and-tell education session with the patient. The DR Score helps me educate and empower patients in their journey to manage their disease with better diet, A1c control, exercise and nutritional supplementation.
In short, the functional ERG findings complement structure. They don’t replace it, but they do help you get a better understanding of which patients are more likely to be stable and which are at greater risk of progressing.
This case was billed using E11.3293 – type 2 diabetes mellitus with mild nonproliferative diabetic retinopathy without macular edema, bilateral based on medical necessity.
Why We Use RETeval
I began using ERG technology during my residency and was later invited to take over as the Chief of Electrodiagnostics by the Oklahoma College of Optometry in 2010. In 2023, we acquired our first RETeval device. We love it because it provides objective functional data that we can take right to the patient, and because the DR Assessment is performed on undilated eyes, the RETeval improves our patient flow. In just a few short minutes, you can obtain objective functional data for both eyes. This information gives me assurance about overall retinal function.
Practice Protocol
I believe an ERG should be done for all patients with diabetes who have:
- Any degree of structural change
- Uncontrolled disease
- Vision changes
- Diabetes for more than 5 years

Nate Lighthizer, OD, FAAO
Northeastern State University (Tahlequah, OK)
Dr. Lighthizer serves in multiple roles as a faculty member of the Oklahoma College of Optometry, including Chief of the Electrodiagnostics Clinic, Director of Continuing Education, and founder and head of the Dry Eye Clinic. He is a founding member of the Intrepid Eye Society, a group of emerging thought leaders in optometry, and currently serves as Vice President. Dr. Lighthizer is a nationally recognized speaker on topics such as advanced ophthalmic procedures, ocular disease, and electrodiagnostics.



