Case study
ERG to Determine Ischemic Status
by Nate Lighthizer, OD, FAAO
When the pieces of the puzzle don’t fit, ERG provides objective functional data to give you the entire picture. In this case, presented by Nate Lighthizer, OD, FAAO, an optometrist and faculty member at the Northeastern State University Oklahoma College of Optometry, the non-invasive Flicker 16 protocol helped to rule out ischemia and save the patient undue stress.
Watch the video of Dr. Lighthizer presenting his case or review the case below.
Patient History
A 50-year-old female presented for punctal plugs. Although she was not scheduled for a retinal evaluation, our resident and a student noticed that the patient’s vision was down in left eye. At this initial exam, her vision was 20/20 OD and 20/24 OS. The patient had a history of diabetes mellitus and was hypertensive. Her last A1C was 8.9 and her blood pressure on the day of her exam was 152/96. Given this, the resident smartly chose to take some photos and perform an OCT.
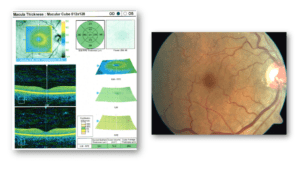
Figure 1 demonstrates what appears to be central serous retinopathy OS. Our typical management for this diagnosis is observation and follow-up in one month for a vision check and repeat OCT. The vast majority of these cases will resolve on their own within a month. Although there were no visual concerns OD, we also took photos and performed OCT on the right eye. Figure 2 shows what appears to be a healthy macula OD.
Figure 1: OCT and Fundus OS
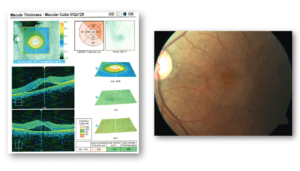
Figure 2: OCT and Fundus
At the one-month follow-up, we see things moving in a good direction in the patient’s left eye, with the pocket of fluid getting smaller (Figure 3). Since we were collecting data on the left eye, we chose to take photos of the right eye as well (Figure 4). Notably, although this was the 20/20 eye, the retina looked different than it did just one month earlier. Now, when we look at the nasal side of the disc, we see noticeable hemorrhages and venus engorgement.
Figure 3: OCT OS
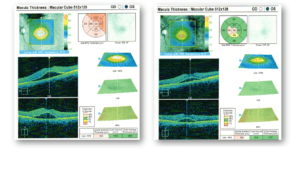
Figure 4: Fundus OS
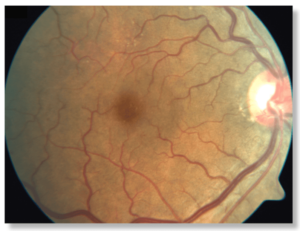
We were still not overly concerned, particularly since this patient still had 20/20 vision OD and the central serous was improving OS, so we scheduled follow-up for one month. At this next visit, the pocket of fluid was still shrinking, and vision was improving OS (Figure 5). But when we took another picture of the right eye, we immediately noticed that the hemorrhaging was getting worse and was now scattered across four quadrants, peripherally, mid-peripherally, and centrally (Figure 6). Interestingly, the OCT in the right eye still looked good (Figure 7). We diagnosed the patient with retinal vein occlusion OD.
Figure 5 OCT OS Figure 6: Fundus OD Figure 7: OCT OD

Why Was the ERG Test Performed?
After consulting with the patient’s primary care physician, the question remained whether we should monitor internally or refer out to a retinal specialist. Depending on your comfort level, either choice is appropriate as long as you can confirm ischemic status using ERG or fluorescein angiography. However, since the latter requires risks associated with injection and ERG is quick, convenient, non-invasive, and far more patient-friendly, we proceeded with a Flicker 16 protocol.
What Were the ERG Findings?
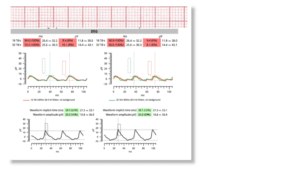
The ERG revealed encouraging findings in both eyes with good amplitude and implicit times, indicating normal retinal functioning and no retinal ischemia (Figure 8). In short, this was a mild non-ischemic vein occlusion.
Figure 8: ERG
How Did the ERG Impact Next Steps?
Together with an OCT that showed no macular edema, the ERG gave us the guidance we needed. With the knowledge that the retina was functioning normally, we had the confidence to say it was safe to monitor this patient closely because there was no ischemia. The patient was a no-show for an appointment one month later, but she returned in 2 months. At that visit, the mild non-ischemic vein occlusion had resolved on its own.
This case was billed using H34.8112 – central retinal vein occlusion, right eye, stable based on medical necessity.
Why We Use RETeval
I began using ERG technology during my residency and was later invited to take over as the Chief of Electrodiagnostics by the Oklahoma College of Optometry in 2010. In 2023, we acquired our first RETeval device. We love it because it provides objective functional data that we can take right to the patient, and because the DR Assessment is performed on undilated eyes, the RETeval improves our patient flow. In just a few short minutes, you can obtain objective functional data for both eyes. This information gives me assurance about overall retinal function.
Practice Protocol
The most common use for ERG in optometric practice is to collect functional information in patients with known or suspected diabetic retinopathy or glaucoma. However, as this case illustrates, ERG has value when assessing patients with many retinal presentations. I believe an ERG should be performed on any patient that has ocular pathology where we need functional information. Specifically, we perform ERG on patients who have:
- Any degree of structural change
- Uncontrolled disease
- Vision changes
- Diabetes for longer than 5 years

Nate Lighthizer, OD, FAAO
Northeastern State University (Tahlequah, OK)
Dr. Lighthizer serves in multiple roles as a faculty member of the Oklahoma College of Optometry, including Chief of the Electrodiagnostics Clinic, Director of Continuing Education, and founder and head of the Dry Eye Clinic. He is a founding member of the Intrepid Eye Society, a group of emerging thought leaders in optometry, and currently serves as Vice President. Dr. Lighthizer is a nationally recognized speaker on topics such as advanced ophthalmic procedures, ocular disease, and electrodiagnostics.



