Case study
Routine ERG Use Supports Complex Patient Management
by Bradley Grant, OD
Subjective functional assessments don’t always yield useful information. Bradley Grant, an optometrist in Shelbyville, IL, utilized his RETeval handheld ERG to determine the appropriate follow-up schedule for a patient with multiple sclerosis, while leveraging the easy-to-interpret, objective functional data to educate the patient on the importance of resuming care with their neurologist.
Watch the video of Dr. Grant presenting his case or review the case below.
Patient history
An established patient presented for a comprehensive exam in 2023. This 70-year-old white female had a family history of diabetes, hypertension and cancer. She was also positive for multiple sclerosis, thyroid dysfunction and high cholesterol. More than ten years ago, she had an episode of optic neuritis in her left eye. Interestingly, relative to her multiple sclerosis, she says she was told that she no longer needed treatment, nor did she need to be seen by neurology. This concerned us given what the Optic Neuritis Treatment Trial (ONTT) tells us about the high likelihood of recurrence in optic neuritis in patients with a history of diagnosis of multiple sclerosis.1-3
The patient’s best corrected vision in the left eye was hand motion. Her vision in the right eye was 20/20. She had mentioned previously that she had a family history of legal blindness, which was somewhat poorly defined; she mentioned glaucoma, cataracts and degenerative disorders of the macula. Before we had access to an ERG, we assumed that this poor vision was related to some form of macular degeneration.
Why was an ERG performed?
The fundus photography showed asymmetry of the optic nerves in terms of pallor (OS>OD) as well as mild cupping and drusen in both eyes (see Figure 1).
Figure 1:
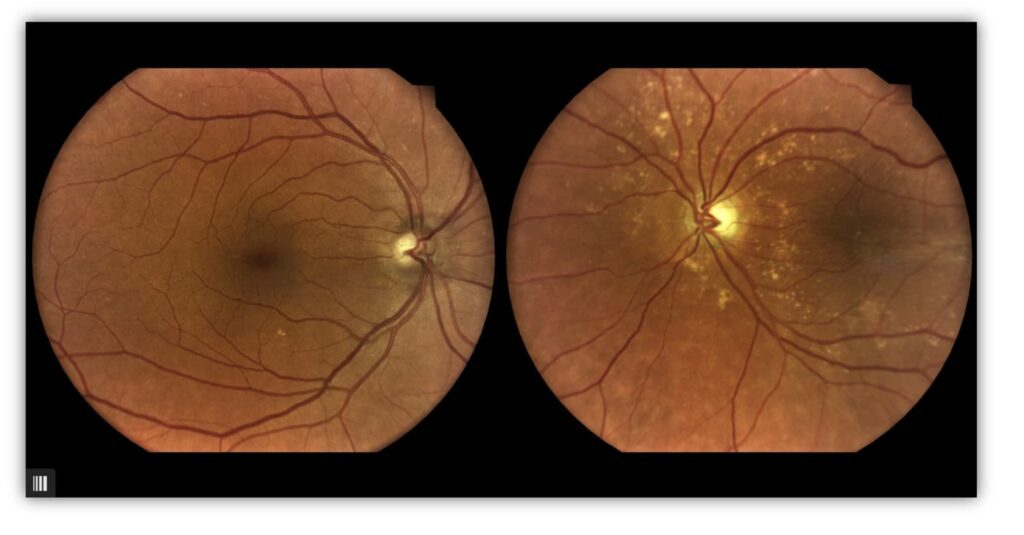
We performed visual field testing, but she routinely failed based on high fixation losses, which greatly underscores the value of an objective functional test. The best VFI we had seen was 21%. OCT showed mild drusen and macular thickening OD and poor fixation and a significant epiretinal membrane OS (see Figure 2).
Figure 2:
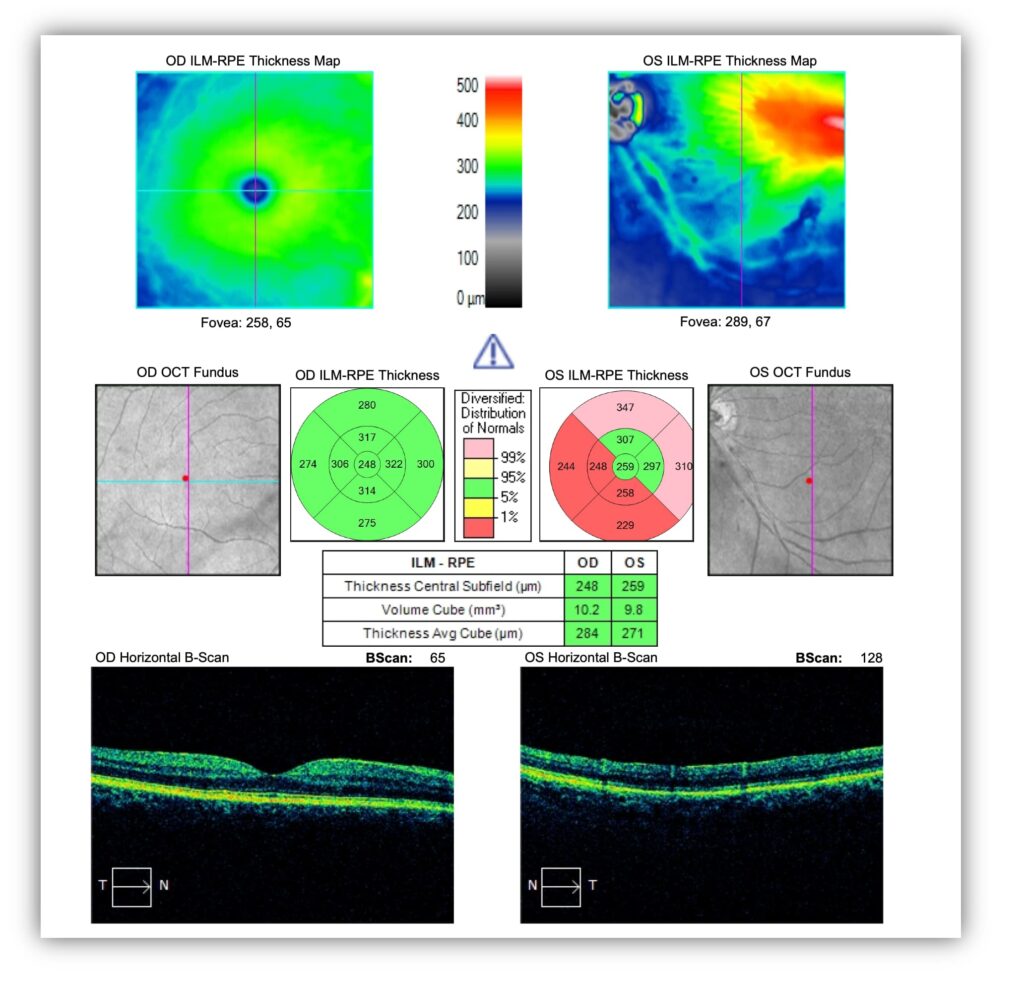
Given her inability to focus on a target straight ahead due to poor vision, even our OCT findings were limited. We had recently acquired the RETeval and had instituted a drusen protocol that prompted the technician to proceed with a Flicker: 16 Td·s test. Although this was not the most useful protocol in this case (PhNR is preferred), it did help provide clarification given the difficulty we were having capturing actionable detail using other tests.
What were the ERG findings?
The results of the Flicker 16 protocol (Figure 3) show the right eye implicit time and amplitude are within normal limits. The left eye’s implicit time is significantly outside normal limits and the amplitude is reduced. These results indicate the presence of cellular stress due to a retinal pathology.
Figure 3:
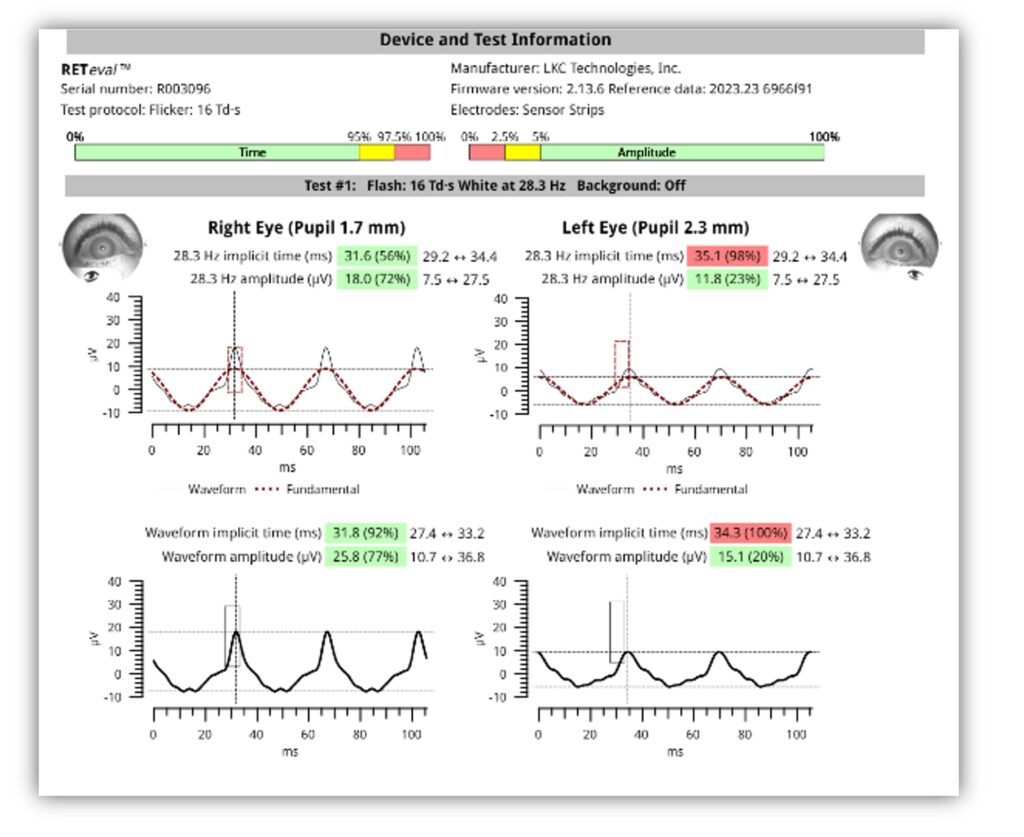
How did the ERG impact next steps?
We are now seeing this patient more frequently to monitor drusen and optic neuritis recurrence. She is scheduled back in 6 months, at which time we will perform the PhNR test. We advised the patient to use an AREDS supplement. We also encouraged her to continue to see neurology, but if she does not, at least we are doing what we can to fill that void.
This case was billed using the following based on medical necessity:
- H35.363 – drusen (degenerative) of macula (bilateral)
- H47.092 – other disorders of optic nerve, not elsewhere classified, left eye
Why We Use RETeval
In 2023, we made the decision to do better for our patients who have diabetes by integrating the RETeval device in our five clinics. We viewed the investment as a necessary step in elevating the level of care that we provide. Prior to adding ERG, our functional assessments were subjective and relied on patient performance and feedback, leaving room for error and poor or unreliable data. We were drawn to the RETeval device because it provides objective, actionable information. We see a high volume of patients and don’t have the luxury of slowing down. Space is also a concern. Many of our instruments take up a full work-up testing room. This portable ERG can be performed in the exam room after the workup, which works seamlessly with our general flow. After performing 1,500 tests, we discovered that it is useful across multiple pathologies, including this case of optic neuritis.
Practice Protocol
Our ERG protocol has evolved. We began by making the decision to obtain a DR Score on every patient who has diabetes. The goal was to test these patients annually, or more often depending upon the level of severity or presence of retinopathy. This protocol applies whether the patient has DR or is newly diagnosed with diabetes. The goal for us is to obtain a baseline exam. We make it standard of care in our practice because we believe it’s what’s best for our patients. In addition to utilizing the DR Score, we routinely use the RETeval device’s PhNR protocol to measure ganglion cell function and aid and support diagnosis, management, and treatment of optic nerve neuropathies, including glaucoma. Finally, we now also perform the Flicker: 16 Td·s protocol on all retinal and macular pathologies, including drusen.

Bradley Grant, OD
Mid-State Eye Partners, Decatur, IL
Dr. Grant is driven by an entrepreneurial spirit and a dedication to providing the highest quality eye care possible. In 2016, he founded Mid-State Eye on the principle that the best service in the eye care business, or any business for that matter, cannot be provided without kindness and compassion for everyone who walks through the door.



